Disruptive Mood Dysregulation Disorder: The Basics
Disruptive mood dysregulation disorder (DMDD) is a condition in which children or adolescents experience ongoing irritability, anger, and frequent, intense temper outbursts.

What is disruptive mood dysregulation disorder?
Disruptive mood dysregulation disorder (DMDD) is a condition in which children or adolescents experience ongoing irritability, anger, and frequent, intense temper outbursts. The symptoms of DMDD go beyond a “bad mood.” DMDD symptoms are severe. Youth who have DMDD experience significant problems at home, at school, and often with peers. They also tend to have high rates of health care service use, hospitalization, and school suspension, and they are more likely to develop other mood disorders.
DMDD can be treated. If you are concerned that your child may have DMDD, schedule an appointment with a mental health professional for a consolation and assessment.
Did You Know?
DMDD is a newly classified disorder, first appearing in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. The DSM is used for the assessment and diagnosis of mental disorders; it does not include specific guidelines for the treatment of any disorder.
What are the signs and symptoms of DMDD?
Children or adolescents with DMDD experience:
- Severe temper outbursts (verbal or behavioral), on average, three or more times per week
- Outbursts and tantrums that have been ongoing for at least 12 months
- Chronically irritable or angry mood most of the day, nearly every day
- Trouble functioning due to irritability in more than one place (at home, at school, and with peers)
Youth with DMDD are diagnosed between the ages of 6 and 10. To be diagnosed with DMDD, a child must have experienced symptoms steadily for 12 or more months.
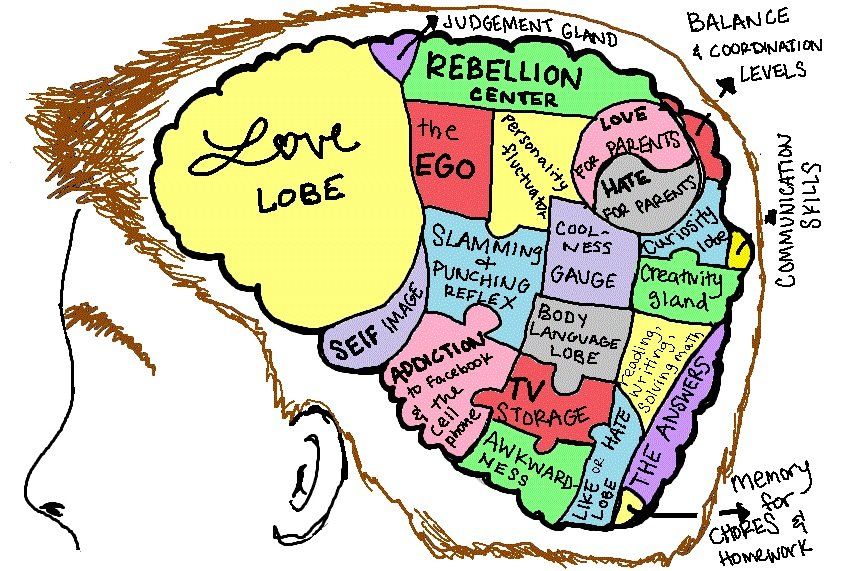
What is the difference between typical irritability and severe irritability?
All children can become irritable sometimes. It’s a normal reaction to frustration. Children experiencing severe irritability (as observed in DMDD) have difficulty tolerating frustration and have outbursts that are out of proportion for the situation at hand. These outbursts occur more often and are more severe than what you would typically expect for children of this age.
For example, a parent tells the child to stop playing a game and do their homework. Any child might be frustrated or annoyed. But a child with DMDD may become extremely upset and emotional and have an intense temper outburst with yelling or hitting. A child with DMDD experiences these intense temper outbursts a few times a week.
Over time, as children grow and develop, the symptoms of DMDD may change. For example, an adolescent or young adult with DMDD may experience fewer tantrums, but they begin to exhibit symptoms of depression or anxiety. For these reasons, treatment may change over time, too.
Children with DMDD may have trouble in school and experience difficulty maintaining healthy relationships with family or peers. They also may have a hard time in social settings or participating in activities such as team sports. If you think your child has DMDD, it is essential to seek a diagnosis and treatment.
How is DMDD diagnosed?
If you think your child may be experiencing symptoms of DMDD, talk to your child’s health care provider. Describe your child’s behavior, and report what you have observed and learned from talking with others, such as a teacher or school counselor. An evaluation by your child’s health care provider can help clarify problems that may be underlying your child’s behavior, and the provider may recommend the next steps.
You also can ask your health care provider for a referral to a mental health professional who has experience working with children and adolescents. DMDD symptoms also can occur at the same time as other disorders associated with irritability, such as attention-deficit/hyperactivity disorder (ADHD) or anxiety disorders. An accurate diagnosis is vital for effective treatment.
For more information about diagnosis and treatment of children and tips for talking to your health care provider, check out NIMH’s fact sheets, Children and Mental Health and Tips for Talking With Your Health Care Provider. If you need help identifying a provider in your area, call the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Referral Helpline at 1-800-662-HELP (4357).
How is DMDD treated?
DMDD is a newly classified disorder, and few DMDD-specific treatment studies have been conducted to date. Current treatments are primarily based on research focused on other childhood disorders associated with irritability (such as anxiety and ADHD). Fortunately, many of these treatments also work for DMDD. NIMH is currently funding studies focused on further improving these treatments and identifying new treatments specifically for DMDD. It is important for parents or caregivers to work closely with their child’s doctor to make treatment decisions that are best for their child.
Treatment for DMDD generally includes certain types of psychotherapy (“talk therapy”) and sometimes medications. In many cases, psychotherapy is considered first, with medication added later. However, at times, providers recommend that children receive both psychotherapy and medication at the start of their treatment.
Psychotherapies
Psychodynamic therapy has been shown to be especially effective for internalizing disorders such as depression and anxiety, as well as in the treatment of emerging personality disorders and in the treatment of children who have experience of adversity. This approach also promotes emotional integration/regulation, and, interestingly, children and teens who engage in psychodynamic psychotherapy tend to demonstrate continued improvement beyond the end of therapy (the so-called “sleeper effect”).
Cognitive behavioral therapy (CBT) and/or Acceptance and Commitment Therapy (ACT) is used to help children and adolescents learn how to cope with thoughts and feelings that contribute to their feeling depressed or anxious. CBT for anxiety often includes exposing the child to situations that make them anxious so that they can learn to respond to those situations better. Clinicians can use similar techniques to teach children to increase their ability to tolerate frustration without having an outburst. This therapy also teaches coping skills for controlling anger and ways to identify and re-label the distorted perceptions that contribute to outbursts.
Researchers also are studying the use of dialectical behavior therapy for children (DBT-C) with DMDD. This type of therapy may help children learn to regulate their emotions and avoid extreme or prolonged outbursts. In DBT-C, the clinician helps children learn skills that can help with regulating their moods and emotions.
It can be effective to combine therapy for the child or adolescent with parent training. Parent training teaches parents or caregivers more effective ways to respond to irritable behavior, such as anticipating events that might lead a child to have a temper outburst and working ahead to avert it. Training also focuses on the importance of predictability, being consistent with children, and rewarding positive behavior.
Medications
Currently, there are no medications approved by the U.S. Food and Drug Administration (FDA) specifically for treating children or adolescents with DMDD. However, health care providers may prescribe certain medications—such as stimulants, antidepressants, and atypical antipsychotics—to help relieve your child’s DMDD symptoms. All medications have side effects. Monitor and report your child’s side effects and review the medications frequently with your child’s health care provider. Visit the FDA website for the most up-to-date information on medications, side effects, and warnings.
- Stimulants are often used in the treatment of ADHD, and research suggests that stimulant medications also may decrease irritability in youth.
- Antidepressants are sometimes used to treat irritability and mood problems that children with DMDD may experience. One study suggests that citalopram (a serotonin reuptake inhibitor antidepressant), when combined with the stimulant methylphenidate, can decrease irritability in youth with DMDD. Please note: Antidepressants may increase suicidal thoughts and behaviors in youth, who should be monitored closely by their health care provider.
- Certain atypical antipsychotic medications are used to treat children with irritability, severe outbursts, or aggression. FDA has approved these medications for the treatment of irritability associated with autism, and they are sometimes used to treat DMDD, too. However, due to the side effects associated with these medications, they are often used only when other approaches have not been successful.
Tips for Parents and Caregivers
Being a parent or caregiver for a child or adolescent with DMDD can be stressful and overwhelming. While working on creating a better environment for the child, you may want to consider the following:
- Learn as much as you can about the disorder. Talk to your child’s health care provider or mental health professional. Ask questions about risks, benefits, and treatment options.
- Talk to your child’s teacher, counselor, or school psychologist. Together, you may come up with strategies, plans, and accommodations that can help your child thrive in school. For more information, check out NIMH’s Children and Mental Health fact sheet.
- Find ways to manage your stress. Take practical steps to manage your own stress to avoid the risk of negative health effects. For tips, see NIMH’s 5 Things You Should Know About Stress.
- Seek additional support and professional help. Parents and caregivers may be able to find resources and encouragement through their local chapter of the National Alliance on Mental Illness, the National Federation of Families for Children’s Mental Health, Mental Health America, and other organizations. (Please Note: These resources are provided for informational purposes only. They are not comprehensive and do not constitute an endorsement by NIMH.)
- Communicate regularly and effectively with your child’s health care provider. Find tips to help you prepare for your child’s visit. For additional resources, including questions to ask your doctor, visit the Agency for Healthcare Research and Quality website.